Working with Heath Benefit Partners
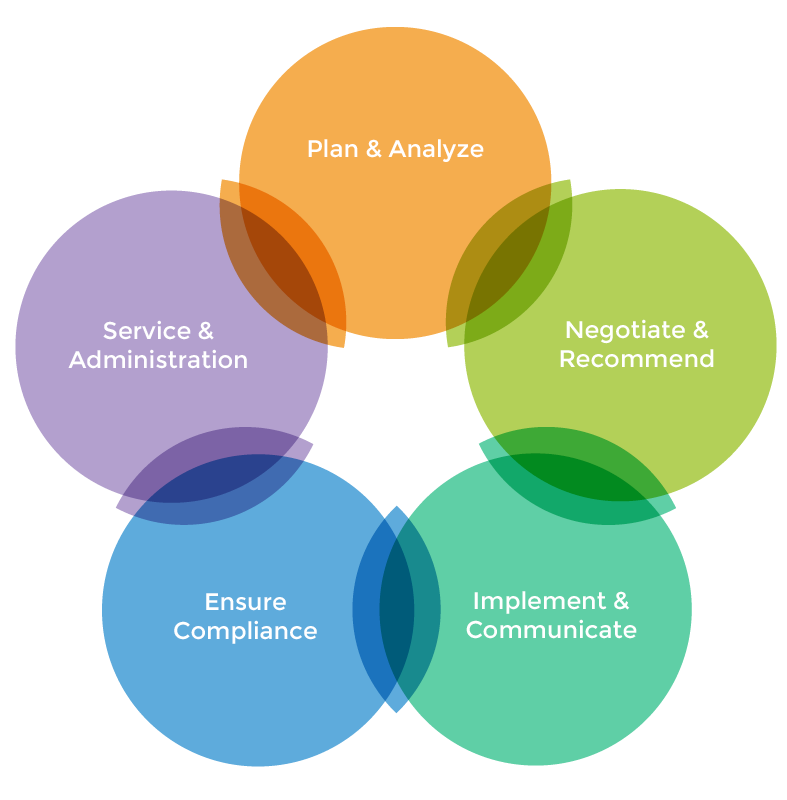
As a broker, not an agent, Heath Benefit Partners works for you and the needs of your organization – not on behalf of any insurance carrier. Our five-step strategic planning and implementation process is based on what large consulting firms do for their Fortune 500 clients. Our strategic planning process is comprised of Step 1 (Plan & Analyze) and Step 2 (Negotiate & Recommend). At this stage, we help you define the objectives you have for your employee benefits program, and we work with the insurance carrier marketplace to meet your goal. Steps 3-5 are all about implementation, compliance, and the kind of ongoing service that makes us an extension on of your HR department for administrative tasks all year long.
- Review current plan performance and analyze needs
- Check Affordable Care Act (ACA) compliance
- Define objectives – outline process for meeting those objectives
- Deploy program modeling tools to maximize your benefits investment while understanding employee utilization impacts
- Benchmark against peer businesses
- Survey employees, if applicable
- Develop and confirm benefits strategy
- Conduct thorough market analysis
- Vet options based on pricing, network, benefits, service and compliance
- Negotiate rate concessions
- Provide custom benefit enrollment literature, education and decision support
- Hold informative employee meetings, health fairs and other educational opportunities
- Provide online access to benefit summaries and enrollment materials
- Offer one-on-one access to benefit specialists
- Provide full service COBRA administration
- Offer ACA, COBRA, HIPAA notifications
- ERISA compliance support
- Complete implementation, administration, and discrimination testing of Section 125 plans
- Provide ongoing legislative updates
- Assist with Form 5500 filing
- Offer patient advocacy to resolve billing, claims, and enrollment issues
- Provide ongoing financial and plan performance analysis
- Access to online resource tools
- Process eligibility, enrollments and terminations year-round

